HYPOTHERMIA.
(Dr. Avalle L. and Dr. D. Marenco)
Introduction .
In this chapter we will discuss a brief history of hypothermia. We will describe the life of Dr. Temple Fay . Shining example of a researcher and as a man whose life was a model of struggle against both physical and moral evil that humanity cannot escape.
The concept according to which Dr. Fay was referring to, was that the cooling of the entire patient it was a cure. And his investigation convinced him more and more that he was right.
Now that the surgery is performed with instruments that were unthinkable in those days, the use of hypothermia is thought of as a technique to be applied to patients who are at risk in the intervention.
We believe that the path taken by this scientist would have to be re-study and re-view wth the clear eyes of scientific research.
Dr. Temple Fay .
Dr. Temple Fay is one of the greats who have opened up a significant section as a pioneer of "total refrigeration" of the human body.
Who with his courage and his determination caused the "breaking of the thermal barrier". This term was mentioned as temperature limit beyond which it is believed that a human being could not survive. The current medical knowledge predicted that a patient undergoing a total cooling was lower than that of natural if a limit. Condition that caused the death of the patient. For this reason it was called "thermal barrier".
We refer to Dr. Temple Fay (Fig. 1 ), one of the most important and qualified neurosurgeons of his time, to which humanity owes a great debt of gratitude.
He was a distinguished scholar and a commendable example of fairness and professional courage.
Fay believed that the temperature of the body is an important pathophysiological factor in certain diseases such as cancer.
The findings of Dr. Fay led to the current therapeutic indications and techniques for hypothermia.
He was also equipped with a tolerance towards the human misunderstanding and this quality of his character to makes even more pleasant and enjoyable study of his life and his works.
Its beginnings.
Temple Fay was born January 9, 1895 in the city of Seattle, Washington. His parents both came from families of great scientists and naturalists. Indicative of the fact that child already, Fay grew up in an academic environment with a great future and high expectations [1,2].
Already from the age of twelve years, Dr. Temple Fay had a clear idea of what would have been his professional destiny. Despite the pressure experienced by his family that he wished for a career in the religious, he followed his vocation and became a surgeon.
He attended the University of Pennsylvania School of Medicine [2].
Fay has spent all his free time on the wards with Dr. William G. Spiller and Dr. Charles H. Frazier, who were well-known respectively as a neurologist and surgeon [1,2].
He started as an assistant to Dr. Spiller and later assisted Dr. Frazier in surgeries to become an assistant instructor in neurology and neurosurgery in [2].
He learned everything you can from them and became a neurologist and neurosurgeon of exceptional ability. He always demanded perfection from the people around him and he acted always with loyalty and honesty [1].
His endless questions and thirst for knowledge have led him to breakthroughs in several areas of neurosurgery and science [3].
His professional life.
In 28 November 1938 Temple Fay introduced for first in the world treatment a total body hypothermia for cancer and brain damage [4].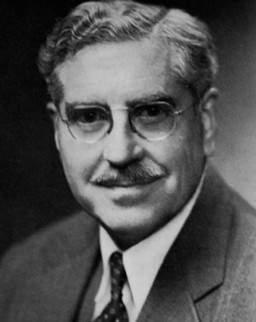 A young woman came to him with an unbearable pain resulting from a metastatic breast for a possible cordotomy.
A young woman came to him with an unbearable pain resulting from a metastatic breast for a possible cordotomy.
He waited, hesitant, several days with the fear of the unknown events, aware of the lessons learned in past on the studies physiological . It was believed that you could not live long subjected to temperatures below 95 F (35C).
Fay finally got the determination to move the project forward.
It was a crisp winter day feature of the climate of Philadelphia. After turning off the fire and closing the door to the corridor, Fay opened all the windows allowing Nature to provide the same cold air that allowed it to maintain a solid 150 pounds of crushed ice on which to lay his patient.
In this experience was used a laboratory thermometer for measuring the temperature rectally because clinical thermometers were not calibrated for temperatures below 94F (34.4°C). Rectal temperature was brought quickly under 90F (32.2°C) and remained so for eighteen hours. Subsequently, the patient was warmed by the heat applied to the body surface and a enema of hot coffee.
Fay commented the unusual treatment with these words: "Within a few hours the patient returned to the levels of consciousness and did not remember the experience."
No nurse wanted to take part and there was a state of mutiny.
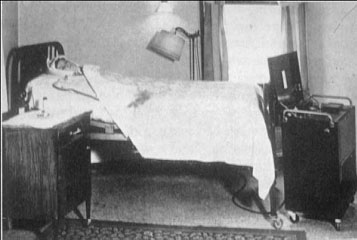
Fay consequently developed a special cooling blanket (Figs. 2 and 3).
He carried out 169 episodes of refrigeration total on human patients eager for relief from intractable chronic pain associated with metastatic malignancies. It was recorded an extraordinarily low mortality (11.2%) and is matched by a highly successful on pain(95.7%) [4].
Fay created an instrumentation capable of cooling within the skull through a direct irrigation using metal capsules, also led a localized hypothermia in the bed of the patient who had undergone a post- craniotomy cancerous . It was then applied routinely to patients with brain abscess , and osteomyelitis of the skull before the advent of antibiotics, a localized cooling through ingenious instruments
.
Regarding patients with severe brain damage , Fay developed a program of hypothermia. The lower rectal temperature reached was 75F ( 23.88 °C) and maintained for three days and the patient recovered completely .
In 1939, data on Fay 's research were presented at the Third Congress on Cancer, the manuscript submitted for publication in Belgium was confiscated by the Nazis.
In the Nazi concentration camps, especially Dachau, these techniques were brutally enforced without the benefit of anesthesia.
The clinical utility of hypothermia was therefore delayed for decades: it was associated with the Nazi atrocities .
Despite the high number of " human subjects" at the disposal of Nazi doctors, the science of hypothermia did not register any progress. Humanity suffered from these facts a period of obscuring scientific and moral .
The Second World War interrupted the "program of human refrigeration," Fay sent his instrumentation Claude Beck and Charles Bailey to help their pioneering work of hypothermia in cardiac surgery [4].
His last days.
Dr. Fay in recent years has turned his attention to the study of mental paralysis and to its rehabilitation [3].
In 1960, after the development of the hypertensive encephalopathy, has retreated into his house to study and write arguments and theses surgery who have him engaged in his busy life [1,3].
The therapeutic hypothermia has become, thanks to its special contribution, part of kit for doctors over the past five years [5,6].
The use of this technique has clearly demonstrated an indicative improvement in a variety of neurological disorders [ 5,8]. This improvement is mainly due to the efforts of Dr. Fay to break the thermal barrier and all other research that men must sometimes confront and break down. Many scholars have continued research of this distinguished physician to whom it is only right to thank [7] .
Over the past 80 years awoke the interest in the hypothermia when it was shown that a slight temperature drop in a patient gave him a clear neuro-protection in a broad category of disorders due to brain damage.
Currently, hypothermia is receiving unprecedented attention from the medical and scientific communities . We will see below (year 2012) measures of each type of dysfunction, or both cerebral heart, made with this technique, solved with great success.

After the Second World War, the liquid nitrogen (-196 ° C) became commercially available. In 1950, this cryogenic fluid has been introduced into clinical practice by Dr. Ray Allington. He used the technique described previously using cotton swabs dipped in liquid nitrogen for the treatment of a variety of neoplastic diseases of the skin (warts, keratoses, and several other neoplastic lesions [9 ]).
In 1958, James Miller from New Orleans and Bjorn Westin from Stockholm conducted a singular clinical study involving ten children severely depressed who had failed conventional methods of resuscitation available for that time [10]. Children in apnea were immersed in a cold water bath built specifically. This operation was interrupted when it happened a spontaneous respiration and rectal temperature approached 27°C.
Young patients were then dried and allowed to warm spontaneously. The minimum temperature of body was between 23 and 30°C and the periods of apnea ranged from 8 to 79 minutes. A checks carried out ten years later, none of the nine surviving children showed neurological problems or cerebral paresis specifications.
In 1958, the extracorporeal cooling, with a pump oxygenating, was successfully used for open heart surgery [11 ]. This operation has been published on the occasion of the first surgical Association of the South, White Sulphur Springs , West Virginia , 10-12 December, 1957.
In this report, the authors argue that a satisfactory open-heart surgery can be done only when the method of cardiopulmonary bypass allows sufficient time for an intracardiac repair deliberate and precise.
Any method that does not allow this expectation must necessarily have a limited application .
From what we have got to check the development of the "techniques of cold "has consistently followed the technological progress that is related to scientific and technical discoveries .
The evolution of physical and engineering medical goes hand in hand.
A final example of how past experiences have become the heritage of the actual surgery, we present a series of works that testify to the true vision of Dr. Fay in regard to this technique that collects great success and is still in a surgical continuous progress and technological.
The hypothermia already introduced in 1938 by Dr.Fay has developed and honed cryogenic surgical techniques and of instrumentation.
At the end of the year 2010 in the world is successfully practiced on young subjects and also the elderly.
In 2010, the Doctors Gunasekaran G, K Bencsath, Hupertz V, Fung JJ, Pettersson G, Miller C. the Cleveland Clinic Foundation, Cleveland, Ohio USA recorded an intervention of deep hypothermia with circulatory arrest on a child to help the management of stenosis of the vena cava as a result of an intervention by the liver. The results were satisfactory [12] .
The following year the Russian team led by Dr. Kazanskaia GM et al.describe the benefits of hypothermia applied to children with the disease of Roger and the reduction of the risks involved [13].
In 2011, the Doctors Krüger T, Weigang E, Hoffmann I, Blettner M, H Aebert, the GERAADA Investigators (GERMANY) describe the cerebral protection during surgery for acute type A aortic dissection: results from the German registry for the type of aortic dissection [14]. A further question comes from researchers of the united states, namely by Drs Lima B, JB Williams, SD Bhattacharya, Shah AA, Andersen N, Gaca JG, Hughes GC.
Who write if the results of the proximal arch replacement with deep hypothermic circulatory arrest, the moderate hypothermia is really justifiable [15]. In contrast, Australian researchers publish a report in which they inform of the first aortic arch replacement without circulatory arrest or deep hypothermia. Matalanis G, RS Koirala, WY Shi, PA Hayward, PR McCall. Are the scholars who have tried that surgical experience [16]. In the same year the University of Malaysia [17] Belgium [18 ] present their work regarding hypothermia, highlighting the undeniable advantages.
In 2012 there are countless operations undertaken in the world. The United States is presented with several aortic operations with hypothermic circulatory arrest [ 19-23]. Also from Greece comes to us, in that year, a publication of aortic surgery with hypothermic circulatory arrest [24] . And two works from Japan on the same topic, attest to the interest in this technique [ 25,26], and research on the improvement of the evoked potential monitoring during surgery of the thoracic aorta in hypothermia [27].
From University of Bologna in Italy the Prof. D. Pacini et al. presents a publication entitled "selective antegrade cerebral perfusion and moderate hypothermic aortic arch surgery: clinical outcomes in elderly patients" [28].
A few months away from China is presented an experimental work on studying the security cerebral on circulatory arrest [29] of a rabbit while the professors Ji B, Liu J, Wang X, C Long, Chineses, compete with the issue of security [30]. The same argument has been proposed by the team of German professors Zierer A, Moritz A. which investigate on the cerebral protection for aortic arch surgery by adopting a mild hypothermia with selective cerebral perfusion [31]. In 2012 at Siena in Tuscany (Italy) was carried out an operation on a child whose body temperature was lowered to 18 degrees Celsius.
Surgeons of Scotte Hospital of Siena stopped his heart for fifteen minutes and started the surgery to remove an big aneurysm from his brain.
The child is seven years old and comes from the province of Caserta. The team that took care of him is made up of twenty surgeons from three different hospitals and was led by neurosurgeon Joseph Oliveri. The child had cerebral ischemia at birth, with the closure of an artery, and subsequently, it has formed a large aneurysm in the brain.
The case has been followed in the pediatric hospital of Siena, was assessed with the heart surgeon Eugenio Neri and neurointerventista Carlo Venturi has created an three-dimensional angiography, with a unit of the latest generation, to identify and assess all the peculiarities of the malformation and the possibility of intervention.
Given the complexity of the case, was excluded both the traditional and endovascular surgery, with the fundamental collaboration of Neurosurgery Meyer Pediatric Hospital of Florence, directed by Lorenzo Genitori of Hospital cardiac of Massa, with staff-led Bruno Murzi. The group of Dr. Giuseppe Olivieri has isolated the aneurysm and Dr. Lorenzo Genitori have revascularized the brain with a very complex operation, using a technique of pediatric neurosurgery for the malformation of blood vessels.
The cardiac surgeons have performed the opening of the chest to cannulate the artery so as to make possible the extracorporeal circulation. It 'an important result for Siena, realized thanks to the excellent diagnostic and interventional and a nice finish for the entire health care system files, with the full synergy created between Le Scotte, The Children's Hospital of Massa and Meyer in Florence.
The child, after a short stay in the Intensive Care Unit Neurosurgery, is admitted in Pediatric Neurosurgery, he's fine.
BIBLIOGRAPHY
1. Murtagh F. Temple Fay, M.D. 1895—1963. Surg Neurol 1991;36:167—9.
2. Henderson AR. Temple Fay, M.D., unconformable crusader and harbinger of human refrigeration. J Neurosurg 1963;20:627—34.
3. Wolf JM. Temple Fay, M.D.—Inquisitive scientist, prolific scrivener. Pathol Med J 1965;68:47—51.
4. Fay T (1959) Early experiences with local and generalized refrigeration of the human brain. J Neurosurg 16: 239–260.
5. Fay T. Intracranial division of glossopharyngeal nerve combined with cervical rhizotomy for pain in inoperable carcinoma of the throat. Ann Surg 1926;84:456—9.
6. Holzer M, Cerchiari E, Martens P, et al. The hypothermia after cardiac arrest study group: mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 2002;346:549—56.
7. Safar P. Mild hypothermia in resuscitation: a historical perspective. - Ann Emerg Med 2003;41:887—8.
8. Safar PJ, Kochanek PM. Therapeutic hypothermic after cardiac arrest. N Engl J Med 2002;346:612—3.
9. Allington HV: Liquid nitrogen in the treatment of skin diseases. Calif Med 1950; 72:153–155.
10. Westin B (1971) Infant resuscitation and prevention of mental retardation. Am J Obstet Gynecol 110: 1134–1138.
11. Sealy WC, Brown IW Jr, YoungWGJr (1958)A report on the use of both extracorporeal circulation and hypothermia for open heart surgery. Ann Surg 147: 603–613.
12. Gunasekaran G, Bencsath K, Hupertz V, Fung JJ, Pettersson G, Miller C. Deep ypothermia with circulatory arrest to aid in the management of suprahepatic vena cava stenosis after liver transplantation. Liver Transpl. 2010 Dec;16(12):1434-6. doi: 10.1002/lt.22183.
13. Kazanskaia GM, Volkov AM, D'iakonitsa TM, Karas'kova AM. [Ultrastructure of coronary microvessels in conditions of heart reperfusion following prolonged ischemia while applying various methods of artificial hypothermia]. Tsitologiia. 2011;53(12):968-77.
14. Krüger T, Weigang E, Hoffmann I, Blettner M, Aebert H. Circulation. Cerebral protection during surgery for acute aortic dissection type A: results of the German Registry for Acute Aortic Dissection Type A (GERAADA). 2011 Jul 26;124(4):434-43.
15. Lima B, Williams JB, Bhattacharya SD, Shah AA, Andersen N, Gaca JG, Hughes GC. Results of proximal arch replacement using deep hypothermia for circulatory arrest: is moderate hypothermia really justifiable?. Am Surg. 2011 Nov;77(11):1438-44.
16. Matalanis G, Koirala RS, Shi WY, Hayward PA, McCall PR. Branch-first aortic arch replacement with no circulatory arrest or deep hypothermia. Thorac Cardiovasc Surg. 2011 Oct;142(4):809-15.
17. Sachithanandan A, Badmanaban B. Re-do sternotomy for complex aortic surgery under deep hypothermic circulatory arrest: left ventricular vent--an invaluable adjunct. Interact Cardiovasc Thorac Surg. 2011 Apr;12(4):608.
18. El Oumeiri B, Louagie Y, Buche M. Reoperation for ascending aorta false aneurysm using deep hypothermia and circulatory arrest. Interact Cardiovasc Thorac Surg. 2011 Apr;12(4):605-8.
19. Khalpey Z, Dekkers RJ, Nauta FJ, Shekar P. Warm beating heart with deep hypothermic circulatory arrest: a technique for an unclampable aorta with aortic valve regurgitation. J Thorac Cardiovasc Surg. 2012 Sep;144(3):731-2.
20. de Zélicourt D, Jung P, Horner M, Pekkan K, Kanter KR, Yoganathan AP. Cannulation strategy for aortic arch reconstruction using deep hypothermic circulatory arrest. Ann Thorac Surg. 2012 Aug;94(2):614-20.
21. Corvera JS, Fehrenbacher JW. Open repair of chronic aortic dissections using deep hypothermia and circulatory arrest. Ann Thorac Surg. 2012 Jul;94(1):78-81; discussion 82-3.
22. Mazzeffi M, Marotta M, Lin HM, Fischer G. Duration of deep hypothermia during aortic surgery and the risk of perioperative blood transfusion. Ann Card Anaesth. 2012 Oct-Dec;15(4):266-73.
23. Di Luozzo G, Griepp RB Cerebral protection for aortic arch surgery: deep hypothermia. Semin Thorac Cardiovasc Surg. 2012 Summer;24(2):127-30.
24. Perreas K, Samanidis G, Dimitriou S, Kalogris P, Balanika M, Antzaka C, Khoury M, Michalis A. Outcomes after ascending aorta and proximal aortic arch repair using deep hypothermic circulatory arrest with retrograde cerebral perfusion: analysis of 207 patients. Interact Cardiovasc Thorac Surg. 2012 Sep;15(3):456-61.
25. Hata M, Akiyama K, Wakui S, Takasaka A, Shiono M. Concomitant aortic valve and ascending aorta replacement with moderate hypothermic circulatory arrest to treat an aortic bicuspid valve with post-stenotic dilatation. Surg Today. 2012 Sep;42(9):913-6.
26. Hiraoka K, Kawatsu S, Mori E, Saiki Y. Total aortic arch replacement using hypothermic circulatory arrest with antegrade selective cerebral perfusion: are there cerebral deficits other than frank stroke?. Gen Thorac Cardiovasc Surg. 2012 Jun;60(6):345-9.
27. Kawaguchi M, Kawamata M, Yamada Y. Improvement of motor evoked potentials monitoring is required during thoracic or thoracoabdominal aortic aneurysm surgery under hypothermic cardiopulmonary bypass. J Anesth. 2012 Apr;26(2):157-9.
28. Pacini D, Di Marco L, Leone A, Di Bartolomeo R, Sodeck G, Englberger L, Carrel T, Czerny M. Antegrade selective cerebral perfusion and moderate hypothermia in aortic arch surgery: clinical outcomes in elderly patients. Eur J Cardiothorac Surg. 2012 Aug;42(2):249-53; discussion 253.
29. Wang Q, Yang J, Long C, Zhao J, Li Y, Xue Q, Cheng L, Cheng W. Hyperoxia management during deep hypothermia for cerebral protection in circulatory arrest rabbit model. ASAIO J. 2012 Jul-Aug;58(4):330-6.
30. Ji B, Liu J, Wang X, Long C. How much is safe: the flow of antegrade cerebral perfusion during deep hyperthermia circulatory arrest. Ann Thorac Surg. 2012 Feb;93(2):693-4.
31. Zierer A, Moritz A. Cerebral protection for aortic arch surgery: mild hypothermia with selective cerebral perfusion. Semin Thorac Cardiovasc Surg. 2012 Summer;24(2):123-6.



