Instrumental and surgical history of the cold.
by Avalle Leopoldo.
Introduction.
Cryosurgery is a surgical discipline, current and rapidly developing, whose origins are lost in time. 3000 years before Christ, the Edwin Smith Papyrus, the oldest medical textbook known to date, dating back to 3500 b. C., makes numerous references to the use of the cold as therapy.
The great scholar and physician Hippocrates pointed out the negative effects of cold on the inhabitants of the lands with cold climates. On the other hand, he has also noted the beneficial consequences of the same to control bleeding and reduce swelling of the affected joint specific [3].
The Hippocratic school of medicine used the total cooling of the body for the treatment of the tetanus [66].
Likewise, the doctors of Hannibal and of Alexander the Great , dipped the sick in cold baths. And, he had did the famous Chinese surgeon Hua To (200 d. C. ) by immersing his patient naked and feverish in a container of stone [66].
Nearly five centuries later , the anesthesia by the cold was known by the Italian doctors [4].
Barron de Larrey , a surgeon in the French army during the Napoleonic campaign in Russia, using the snow and ice cooled the parts that were to undergo amputation to make the pain-free procedure [5].
This information is purely descriptive and, if you do not make an effort of imagination, there comes to mind any " instrumental device " that may have been used in the past.
Writes rightly prof. Korpan:
"From the check of the history of cryosurgery we see that she has progressed in leaps and each jump is usually activated by technological innovations that immediately preceded it."
And it is precisely the evolution of cryosurgical instrumental, which evolved like to "leaps" because the progress of physics and science in general develop like a "explosion" after a relative period of stagnation.
We can say that thanks to the discovery of the thermometer from Fahrenheit invented in 1714 and reinvented by Reaumur and Celsius that cryosurgery was equipped with a real "scientific" instrument.
And this is the date by which, in our opinion, it ends the cycle of use of cryosurgery as empirical method that we have defined about the instrumental part as the "Instrumentation CRYO-ARCHAIC".
It ends the period of CRYO-ARCHAIC instrumentation and is born what of the "CRYO-TECHNICAL instrumentation".
In 1961, Irving Cooper developed the first closed system of cryoprobes and we are entered the modern era of cryogenic surgery. He begins the period which we define as of the " CRYO-MODERN instrumentation" giving end to the period of CRYO-TECHNICAL instrumentation. This period lasts until the present day with ups and downs of success and long periods of stasis almost flat inactivity (at least from the point of view of creation of new instrumental methods ). We believe that by 2015 it will start the phase of the Cryosurgical instrumentation of the FUTURE.
Based on the above classifications we will set our research on the development of the Cryosurgery instrumentation namely:
1 - ARCHAIC period of the cryo-instrumentation.
2 - TECHNICAL period of the cryo-instrumentation.
3 - MODERN period of the cryo-instrumentation.
4 - FUTURE period of the cryo-instrumentation.
Please note that the timing of the development of the Cryo-instrumentation adopted by us is based on concepts purely arbitrary.
The degree Fahrenheit is the unit of a scale for measuring the temperature named after the German physicist Gabriel Fahrenheit.
Both the Greeks and the ancient Egyptians were wont to apply cold compress on wounds or head injuries to treat or to soothe the pain.
Hippocrates cured tetanus immersing the patient in a bath frosty. 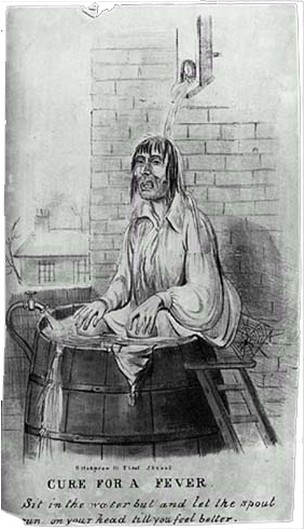 Recall that the doctors of Hannibal and of Alexander the Great, at times, their sick subjecting them to a cold bath. As the famous Chinese surgeon Hua Tt
Recall that the doctors of Hannibal and of Alexander the Great, at times, their sick subjecting them to a cold bath. As the famous Chinese surgeon Hua Tt
made in 200 d. C. We met earlier Napoleonic Barron de Larrey the surgeon, who during the military campaign in Russia, used packs of snow and ice, to cool the parts that must undergo amputation. This treatment rendered the procedure pain-free (or almost). We can continue with these ancient examples of applications of the use of cold, but we cannot find, surgical instruments, except that clothing or bandages cooled with ice or snow.
It was used ice packs produced by nature or snow.
In some cases, the patient was forced to plunge into cold baths or to undergo cold showers.
Knowing how to read between the lines, in all likelihood, the doctors tried to get the cold in every way. This their research could have been a stimulus to physicists or engineers. These, however, are only hypotheses that we formulate without any historical reference.
The following image, in its irony, reveals many truths that to a careful observer are more eloquent than many words.
There are not tools that indicate the temperature of the patient or that of the bath. Hygiene is not exactly what doctors of our day would have allowed. And the state of the patient may be questionable for the treatment it receives.
And it is the invention of the thermometer that will allow doctors to make assessments and make changes to the systems that they use. With this tool ends the archaic era of cryosurgical instrumentation and start that technique

TECHNICAL PERIOD OF OF CRYO-INSTRUMENTATION.
James Arnott.
J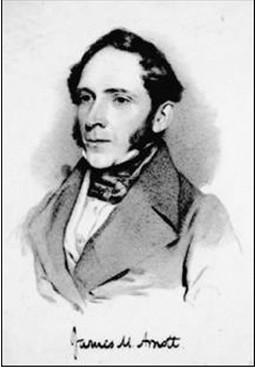 ames Arnott (1797-1883) between 1845 and 1851, an English physician of Brighton (Figure B), was the first person to use the extreme cold locally for to tissue destruction. In 1845, he described the use of iced saline solutions (about -20°C) by freeze advanced cancers in accessible sites, with a consequent reduction in tumor volume and improvement of local pain and bleeding [8] [Bird, 1949]. The tumors treated by Arnott using the technique of freezing including breast cancer, uterine cancer, and certain skin cancers. Although the palliative care was the main goal, he recognized the potential of cold for the treatment of cancer. He advocated treatment with low temperatures for acne, neuralgia, headache, reaching a temperature of -24°C. He also designed a device for the application of cold in surgery, an instrument that was presented at the Great Exhibition in London in 1851. [3]
ames Arnott (1797-1883) between 1845 and 1851, an English physician of Brighton (Figure B), was the first person to use the extreme cold locally for to tissue destruction. In 1845, he described the use of iced saline solutions (about -20°C) by freeze advanced cancers in accessible sites, with a consequent reduction in tumor volume and improvement of local pain and bleeding [8] [Bird, 1949]. The tumors treated by Arnott using the technique of freezing including breast cancer, uterine cancer, and certain skin cancers. Although the palliative care was the main goal, he recognized the potential of cold for the treatment of cancer. He advocated treatment with low temperatures for acne, neuralgia, headache, reaching a temperature of -24°C. He also designed a device for the application of cold in surgery, an instrument that was presented at the Great Exhibition in London in 1851. [3]
On Christmas Eve of 1877, Cailletet, French, and Picet, Swiss, have [1878] demonstrated at the French Academy of Sciences that oxygen and the carbon monoxide can be liquefied under high pressure. The following year, 1878, the Pictet [1878] has also documented the liquefaction of the oxygen, using a cascade mechanics refrigeration . In 1895, it was the first time that Carl von Linde, German, managed to liquefy the air compressing it and then leaving it to rapidly expand, and so that he has produced liquid air. He has promoted its spread in Europe and the United States. (1895 - 1896).
In 1898, Professor Charles E. Tripler of Columbia University has developed a method based on liquid air, and persuaded the New York dermatologist, Dr. A. Campbell White to use this cryogen in the treatment of skin lesions.
The first clinical application of liquid air ( -190°C ) took place in 1889 for the work of a doctor in New York City, Campbell White, who used a tampon, a spray, or a roller device in brass. The first publication of Dr. White was entitled "Liquid Air in Medicine", and appeared on The Medical Record, July 22 [9].
Have been used several techniques. The two most frequently used were the method to "buffer" and the "spray". The "buffer" consisted of a small amount of cotton wool wrapped
around the end of a stick of wood that could be pointed, flat, round, or in the shape of a paddle on the extent of the lesion to be treated. This was immersed in the air and liquid applied to the skin lesion.
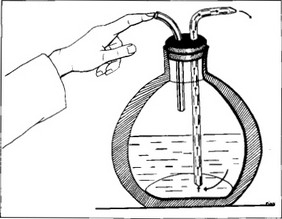
The spray is obtained by inserting a particular rubber stopper perforated containing two glass tubes in an ordinary washing container, and closing with a finger the mouth of the inlet tube (Fig. C ).
The spray has been used topically for pain relief and the treatment of dermatological disorders such as "poison ivy", dermatitis, herpes zoster, boils, carbuncles, lupus vulgaris, and lupus erythematosus.
The Dr. White has performed a controlled experiment in the treatment of poison ivy dermatitis: "A band around the forearm approximately three inches wide was slightly frozen The solidified carbon dioxide (-78.5°C) has been introduced in clinical practice by Dr. William Pusey of Chicago. Which has favored the use of solid carbon dioxide, which was commonly used as a refrigerant. He has treated, vascular nevi, lupus erythematosus, lupus vulgaris, and epithelioma [10].
In addition to these initial reports, many physicians made use of freezing techniques in dermatology.
After 1910, the liquid air was used rarely, and the solid carbon dioxide cryogenic agent became the most popular in the early 1900s.
with the spray, then the treatment was applied to the entire surface including the poisoned that had been treated with the air in the next dressing".
Late 19th century: the use of liquid air.
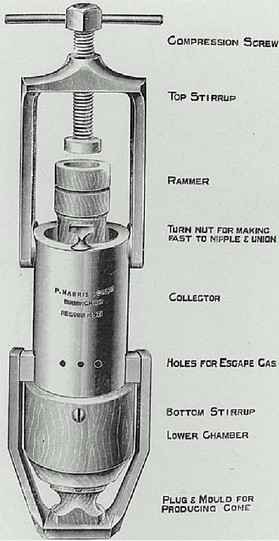 It is still a British doctor who has had the merit of "groped" an instrumental approach to the application of cryosurgery. His work is the effort to use the "mechanical technology" to improve the cryosurgical approach. The gas (or cryogenic liquids) were essentially ready and available to surgeons but they are used tampons, spray, brass rollers, spray bottles or cotton balls. Let's talk about Hall-Edwards [1913] of Birmingham, United Kingdom, which is primarily known for his manifold compressor of carbon dioxide created in 1911.
It is still a British doctor who has had the merit of "groped" an instrumental approach to the application of cryosurgery. His work is the effort to use the "mechanical technology" to improve the cryosurgical approach. The gas (or cryogenic liquids) were essentially ready and available to surgeons but they are used tampons, spray, brass rollers, spray bottles or cotton balls. Let's talk about Hall-Edwards [1913] of Birmingham, United Kingdom, which is primarily known for his manifold compressor of carbon dioxide created in 1911.
In his monograph he wrote later, in 1913, he detailed the use of carbon dioxide for the treatment of many conditions, in particular, rodent ulcers. He proposed the use of cryosurgery with the help of X-rays. His studio has brought a great contribution to the cryosurgery opening roads to future research methodologies that will be the strong point of this science in the years to come. At the same time, Cranston-Low [1911], Edinburgh physician in the department of dermatology, has confirmed, highlighting on an experimental basis, that the use of carbon dioxide snow, was effective in "thrombosis, direct damage to the tissues, and exudates inflammatory".
In subsequent years, the carbon dioxide snow has been very successful it was used for a variety of benign conditions of the skin and it remained popular until the 1960s
During this period, several devices have been developed for the use of carbon dioxide snow. For example, Campbell White has designed a roller for the treatment of erysipelas (Rubinsky, 2000) [67]. The great advantage of the liquid air was that it was easy, through it, to get the low temperatures, allowing you to operate the tumors, but a disadvantage is the difficulty of transportation. Sir James Dewar has solved this problem by allowing the transport and storage inventing a container formed by two glass walls with a vacuum between them (Gage, 1998; Rubinsky, 2000) [6, 67]. Even today, the containers used for the refrigerants have about the same design.
Dr. Temple Fay . Talking about the history of instrumentation Cryosurgery you cannot omit of describe the work of one of the greats who have opened an basic paragraph of this science. The man who first started as a pioneer the "total refrigeration" of the human body. Who with his courage and his determination caused the "breaking of the thermal barrier." With This term was mentioned the thermal limit in which it was believed that a human being could not survive. The current medical knowledge, in those days, predicted that a patient undergoes a total cooling lower than it was the natural limit can cause the death of the patient. For this reason it was called "thermal barrier". We refer to Dr. Temple Fay (Fig. E), one of the most important and qualified neurosurgeons of his time, to which humanity owes a great debt of gratitude. He was a distinguished scholar and a commendable example of fairness and professional courage. Fay believed that the temperature of the body is an important pathophysiological factor in certain diseases such as cancer. The findings of Dr. Fay led to the current therapeutic indications and techniques for the hypothermia. He was also equipped with a tolerance toward the human incomprehension and this makes even more pleasing to the study of his life and his works.
Talking about the history of instrumentation Cryosurgery you cannot omit of describe the work of one of the greats who have opened an basic paragraph of this science. The man who first started as a pioneer the "total refrigeration" of the human body. Who with his courage and his determination caused the "breaking of the thermal barrier." With This term was mentioned the thermal limit in which it was believed that a human being could not survive. The current medical knowledge, in those days, predicted that a patient undergoes a total cooling lower than it was the natural limit can cause the death of the patient. For this reason it was called "thermal barrier". We refer to Dr. Temple Fay (Fig. E), one of the most important and qualified neurosurgeons of his time, to which humanity owes a great debt of gratitude. He was a distinguished scholar and a commendable example of fairness and professional courage. Fay believed that the temperature of the body is an important pathophysiological factor in certain diseases such as cancer. The findings of Dr. Fay led to the current therapeutic indications and techniques for the hypothermia. He was also equipped with a tolerance toward the human incomprehension and this makes even more pleasing to the study of his life and his works.
His endless questions and thirst for knowledge have led to breakthroughs in several areas of neurosurgery and medicine, looking for new and innovative methods for the development of his science [15].
In 1939, data on the research of Fay were presented at the Third Congress on Cancer, the manuscript submitted for publication in Belgium was confiscated by the Nazis.
 In the Nazi concentration camps, especially Dachau, these techniques were brutally enforced without the benefit of the anesthesia.
In the Nazi concentration camps, especially Dachau, these techniques were brutally enforced without the benefit of the anesthesia.
The clinical utility of the hypothermia was therefore delayed for decades: it was associated with the Nazi atrocities.
Despite the high number of "human subjects" at the disposal of Nazi doctors, science of the hypothermia did not register any progress. Humanity suffered from these facts a period of obscuration scientific and moral.
The Second World War interrupted the "human refrigeration program", Fay sent his instrumentation to Claude Beck and Charles Bailey to help their pioneering work of the hypothermia in cardiac surgery [16].
After the Second World War, liquid nitrogen (-196°C) has become commercially available. In 1950 this cryogenic fluid has been introduced into clinical practice by Dr. Ray Allington.
The pioneering work in the 50s on a total deep hypothermia for neurological protection during cardiovascular and neurosurgical procedures has introduced the hypothermia in neurosurgical modern clinical practice [13-14]. Also in 1958, the extracorporeal cooling, with a pump oxygenating, was successfully used for open heart surgery [12]. This intervention has been published on the occasion of the first surgical Southern Association, White Sulphur Springs, West Virginia, 10-12 December 1957.
The necessity of oxygen decreases in hypothermia and what becomes the basis for which the body tolerates circulatory occlusion [1]. The oxygen demands of the body in hypothermia may be provided by a simple extracorporeal oxygenator with a pump at low flow rate to obtain a time resolved of intervention and a intracardiac consumption [2,3].
Speech which a prelude to the modern period of Cryo instrumentation.
Since the beginning of the century in 1900 (XIX ) until the 1960s the evolution of instrumental cryosurgery had not a great development.
The doctors, were limited to cool for "contact" cotton balls or cloth for compresses, in the best of cases, objects of copper or other metals.
The dr. Arnott, exceptionally, designed a device for the application of cold in surgery, an instrument that was presented at the Great Exhibition in London in 1851. That apparatus, according to the doctors of the period, was complex and artificial. He did not have the expected success.
Meanwhile the cryogenic liquids were essentially available thanks to the work of Linde, to the surgeons but were used with tampons, sprays, rollers of brass, spray bottles or cotton balls.
The physics had already found the streets to explain the use of this technique to achieve its maximum efficiency (see the research Onnes), however, the medical world was not yet ready.
From the instrumental point of view, there was an exception, let's talk about Hall-Edwards [1913] of Birmingham, UK, who created a compressor manifold of carbon dioxide in 1911 (Figure D).
In the early 60s the modern Cryosurgery began through the collaborative work of a doctor, Irving Cooper, and an engineer, Arnold Lee [18].
This union between a doctor and an engineer was the winning factor that has paved the way for the cryosurgery understood in the current sense of the term. It is, then, thanks to Dr. Lee Cooper and the engineer Arnold Lee that the medicine has been enriched by a very effective tool by opening the way for modern interventions in the field. It is a probe that became the prototype from which they were built and designed the cryoprobes later. It was a probe which worked with liquid nitrogen.
PERIOD MODERN OF CRYO-INSTRUMENTATION.
Irvin Cooper and the cryogenic surgery.
In 1961 , the neurosurgeon Irving Cooper (Fig. G) developed an automated cryosurgical apparatus which used liquid nitrogen circulated through a sheath isolated metal. He was the first probe system closed cooled with liquid nitrogen ( -196 ° C ), which ushered the modern era of the cryosurgery [18]. Although the apparatus has been designed to produce a cryogenic lesion in the brain for the treatment of Parkinsonism, the interest in the cryosurgery clinical has blossomed after its development.
Cryosurgery then began to be used to treat tumors at different sites [6]. In 1963 important applications of cryosurgery in the treatment of Parkinson's disease had followed, Cooper (1963) suggested that primary and metastatic tumors of the liver could be treated with the cryosurgery and that freezing could produce an immunizing effect, anticipating of several decades biological discoveries really fundamental. Between 1960 and 1970 many experiments of cryosurgery were made to treat cancerous cells, many of which were carried out on various types of animal and in vitro. Cooper had noted that the cryolesions formed in situ were limited and were gradually absorbed by the body which is reducing, within 6-8 weeks after the procedure, to fibrotic scars.
Dr. Cooper has helped to restore muscle function of thousands of victims of Parkinson's disease, through a surgical technique that has developed in the early 1950s.
The procedure consisted in destroying the lowest parts of the brain involved to stop the flow of blood to the cells that have been the transmission of the disease.
The cryotherapy, therefore, as a therapeutic technique had received a great stimulus from the introduction of the first instrumental cryosurgical system. It was capable of transporting liquid nitrogen (-196°C ) to the tip of probes whose rod, subjected to high isolation, allows to it, built of very conductive metal, to reach the low temperatures.
The system was the result of the collaborative effort of Irving S Copper, a neurosurgeon, and Arnold Lee, engineer [18]. Their probe has been the prototype from which all future cryosurgical probes that use liquid nitrogen have been developed [6]. This apparatus allowed the surgeons for the first time to treat deep lesions in parenchymal organs , with minimal trauma to the rest of the organ.
The development of intraoperative probes and their use to monitor the process of freezing tissue has made to rise interest in the cryosurgery in the 90s. This renewed interest was very evident in the treatment of prostate and liver cancers with cryotherapy. The rapid advances made in the techniques of imaging intracranial had offered a new interest to treatment of brain tumors [6]. We note that Gage and co-workers in 1982 showed that the great vessels tolerate freezing without breakage. The cryosurgery then began to be used for cancers of the skin, lung, breast, prostate, bowel and pharynx. The first attempts to destroy tumors of the liver used the direct application of liquid nitrogen on the surface of the liver (Orpwood, 1981; Bischof et al., 1993).
The cryosurgery then began to be used for cancers of the skin, lung, breast, prostate, bowel and pharynx. The first attempts to destroy tumors of the liver used the direct application of liquid nitrogen on the surface of the liver (Orpwood, 1981; Bischof et al., 1993).
Dr. Irving S. Cooper, died of cancer a Wednesday in Neapolis, Florida. He was sixty-three years old and lived in that city.
The due recognition to this scientist, admirable and ingenious, it is never enough.
The streets that his laudable intuition has opened only now are beginning to be understood and appreciated.
In the time interval between the years 1961 and 1970, many scholars in the footsteps of Cooper, attempted the construction of apparatus for cryosurgery utilizing various cryogenic gases. Was tried liquid nitrogen and other agents, including nitrogen oxide, carbon dioxide, argon, ethyl chloride, and fluorinated hydrocarbons [26].
In 1965, Dr. Douglas Torre, a leading dermatologist , he used the device of Cooper to treat diseases of the skin. He allowed for the development of a spray device that operates with nitrogen which was able to be also used with cryoprobes of various shapes and sizes. He converted the open line by a conduit to the outside in a closed system.
The results of the treatments Cryosurgical were similar to those obtained with the apparatus with liquid nitrogen of Cooper.
The Dr. Torre treated many types of basal cell carcinomas and squamous with the cryosurgical technique.
Dermatologists practice this science for about seventy years. In several types of skin lesions is the treatment of choice, and in many others, an alternative method of therapy. It is a simple, safe, fast, effective and relatively painless technique which offers excellent aesthetic results. Thanks to its special characteristics of lower risk of infection and bleeding, the cryosurgery is ideal in the treatment of patients with increased surgical risk, such as diabetics, hemophiliacs, or patients receiving anticoagulants.
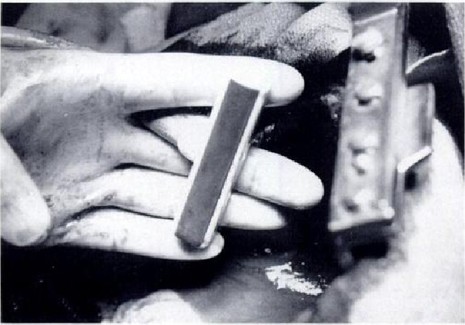
The Dr. S. Zaccarian A. and MT Adham, [17] in 1966, they prepared an alternative method inexpensive and simple to use. They shaped copper discs of one inch thick with a diameter of 0.5-3 cm that could be mounted on a plastic handle. These were immersed in liquid nitrogen to about -196°C, and applied it to the skin.
In 1967 Setrag Zacarian introduced a manual of self-pressurization .
The following year, he reports that the project activity of an engineer, Michael Bryne, contributed to the creation and development of a portable device to spray with liquid nitrogen.
After some modifications, this unit became the first commercially available device of cryosurgery handheld.
Thus we see that, after the experience of working with an engineer to Cooper, the creation of devices became more and more effective and functional in current use.
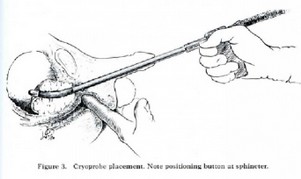
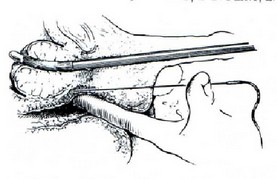
Gonder changed, therefore, the apparatus of Cooper and was the first to use it for prostate diseases [20].
These publications stimulated an immediate interest of the urologists and developed an intense experience with the cryosurgery of the prostate [21-24], including, as mentioned above, a perineal approach from the glans made by Flocks et al. in 1972 [25].
In the late 60's many surgeons will be challenged in cryosurgery of the prostate according to the experience and suggestions of Gonder. (Fig. U, Fig V).
With the availability of cryosurgical equipment, says Dr. Pope, to have been able to repeat the work of Gonder and his associates in the prostate of the dog and then in the prostate of man.
Towards the end of the 60 years the surgeons, at least those Americans, regarding the remediation of prostate cryosurgery, they abandoned the technique of Gonder preferring endoscopic surgery using local anesthesia.
It is the beginning of a new approach in the search for methods increasingly safer and generalizing that will lead, after some trial and error, to modern prostatic cryosurgery

CRYOSURGERY OF YEARS 70 and 80.
In the early 1970s the cryosurgery undergoes a dramatic arrest. The inability to be able to follow the development of the cold front in the tissues undergoing treatment prevents a safe and controlled operation.
Only the cryosurgery of the skin and that of the externally accessible organs has survived.
Accordingly There are few construction companies that design and create prototypes that have no commercial future.
A representative example is the creation of two instruments, an ophthalmic said "crioestrattore" (Fig. H) and the other as a probe Cryo appointed "multicrio" (cryopencil).
Their basic function was a high operational efficiency and a small footprint. You could carry it in a handy bag.
 These two tools, patented, were built in Genoa ( Italy ) thanks to the expertise of engineers and professors from the University of Genoa.
These two tools, patented, were built in Genoa ( Italy ) thanks to the expertise of engineers and professors from the University of Genoa.
The operational convenience and the slenderness of intervention made them particularly efficient and equipped with features which, in some respects, still could have been appreciated at present.
Still in the early 1970s precisely in December of 1972, Dr. R. H. Flocks public on the Journal of
Urology an interesting article describing an operation of perineal prostatic cryosurgery . It is, in our opinion, a further step towards the modern cryosurgery [25]. The work carried out at the Department of urology, University of Iowa Hospitals, Iowa City, Iowa. The researchers, susceptible to the immunizing effects of the interventions of cryosurgery , show that Dr. Soanes and collaborators have postulated a cryoimmunity because two patients with metastatic cancer have had a regression following this type of operation [19]. Laboratory research on autoantibodies from accessory sex glands and seminal vesicles of rabbit after freezing have supported this hypothesis [27].
Dr. Flock shows that its purpose is to determine the effects of the cryosurgery applied perineal in patients with prostate cancer. He informed that his attempts were as follows:
1 ) indicate the effectiveness of cryosurgery in destroying the local lesion, while maintaining the
integrity of the bladder and urethra adjacent;
2 ) determine whether the immune response was a quantitative phenomenon in this research
of the prostate and check if it would have been more issued for the stimulation of
the production of autoantibodies and to recognize if it takes any clinical change
(which is the regression of metastases).
The Dr. Flock from excellent surgeon had proposed a very sensitive research goal, a goal that only after several years of biological investigations has been partially elucidated. (see our chapter on the history of the Cryobiology ).
In the years 1975, 1976, Prof. Gage published two reports on cryosurgery interventions of the skin.
The title of the first work was published in September 1975: " Cryosurgery for difficult problems of skin cancer" [33].
The author begins with these words: "I will defend this therapeutic technique as his own lawyer and I will describe the benefits that justify its use in certain skin cancers". Cryosurgery has developed a wide range of nominal value. The vast experience of the prof. Tower and of the prof. Zacarian has shown that almost every type of skin cancer can be successfully treated by freezing in situ. They clearly showed the advantage of the ease and simplicity in the cryosurgical treatment of common cancer of the skin.
In the intervention the Dr. Gage describes that were used cryosurgical apparatus using liquid nitrogen that can be handled either as a closed system employing cryoprobes or by a jet of liquid nitrogen directly onto the fabric. With a cryoprobe, the method is to apply the cryoprobe to the tumor making them reach the desired temperatures.
The second work, published in 1976 was titled: "Five-year survival after cryosurgery for oral cancer".
They are described in the interval from 1964 until 1970, the intervention of six selected patients with oral cancer who were treated with the cold in situ with the intent to cure the disease.
The author points out that recent results demonstrated the suitability of the method applied to high-risk patients.
This technique allowed, among other benefits, to avoid operations sacrifice and risk for the bones.
Statistics of five-year survival showed that cryosurgery has been used most successfully on small and medium-sized tumors without cervical lymphadenopathy. The results justify the continued use of the cryosurgery in carefully selected patients.
In the 70s, after a renewed enthusiasm of the previous years, some uses of the cryosurgery fell into disfavour, others were preserved with less importance, and others recorded in the textbooks as specific techniques. One of the first to fall into disuse was cryosurgery for Parkinson's disease, which had been the original stimulus of Cooper and his colleagues. This change was not due to the fault of the technique. On the contrary, in the years 1963-70, Cooper and his colleagues, S. Stellar and J. Waltz had made a stereotactic cryosurgery of basal ganglia in approximately 8000 patients with the characteristics of tremor and rigidity of Parkinsonism; the benefits were found in 85 to 90% of these patients [28]. However, when L-DOPA was in use in 1968, the stereotactic cryosurgery was no longer necessary in most cases. But a minimum interest in the treatment of intra-cranial tumors and cerebrovascular abnormalities continued [29,30].
The use of the cryosurgery for prostatic diseases fell into disuse because the extension of the drainage catheter requires another operation, the incidence of complications, and the effectiveness of transurethal resections.
Some interests persisted in the treatment of prostate cancer because of the potential benefit may be due to the favorable immunological response as suggested after the prostatic cryosurgery [ 31,32 ]. The competition of the laser has reduced the use of the cryosurgery of gynecological diseases (chronic cervicitis intra-epithelial neoplasia and cervical), but both techniques had their supporters. Cryosurgery Dermatology, commonly used with simple cryoprobes with liquid nitrogen, it became accepted [33-35].
The techniques of cryosurgery became commonly used in ophthalmology for the treatment of various diseases including cancers [36,37]. The use of cryosurgery for skin diseases continued to increase as evidenced by the sponsorship of the American Academy of Dermatology in teaching courses in its annual meetings. Cryosurgery in cervical intraepithelial neoplasia and chronic cervicitis continued and was considered standard therapy, although was competitive with the laser [38-42].
Cryosurgery for endobronchial disease has become a usual technique in the world.
Dr. Sumida Sajio and colleagues [43-47] described the results of cryosurgical treatment on the basis of the last forty years of experiments and clinical. The observations in vitro and in vivo formation of ice extra and intracellular and the failures of the microcirculation dependent disseminated intravascular coagulation after freezing in situ were recorded in detail by Professor Sumida and collaborators since 1970 [48,49].
Cryosurgery for cancer is increased with the combined use of chemotherapy. In other areas, progress was slow. The use of the cryosurgery for the treatment of hemorrhoids had lost favor because of the simplicity of the techniques of injection ( injection) and banding ( bandages ). The liver tumors were treated by cryosurgery, but not being able to see the depth of the lesions allowed only occasional clinical applications and from this he obtained an uncertain benefit. The interest for cryosurgery regard to prostate cancer was maintained in some medical centers what is highlighted in a series of publications by Bonney et al. which showed a favorable return as compared to other therapies [50,51].
In 1988 Tower, and Lubritz Kuflik were co-authors of a book on the practical aspects of cryosurgery in dermatology [11].
Thanks to these scholars in recent years, cryosurgery became an established standard treatment for a wide variety of benign and malignant skin lesions, with new uses described in this report.
The most important event which was been the fulcrum around which began to act cryosurgery was the discovery of the use of ultrasound (U.S.) in the detection of cold fronts in the prostate interventions.
This is due to the ingenious discovery that Dr. Onik, with two publications, one published in 1985 and another, three years later in 1988, became evident and demonstrated the effect detector of sound waves in the ultrasonic frequency [52-53].
The experiments were performed on five dogs and, given the fundamental importance and the future consequences made to cryosurgery, we focus briefly on the main details of the image.
The title of the publication in 1985 is: "Sonographic monitoring of hepatic cryosurgery in an experimental animal model." [52].
The author reports that the ultrasound was used in real time to monitor the evolution in vivo of hepatic cryolesions induced in four mongrel dogs.
The results suggest that the ultrasonic technique is therefore an efficient and accurate means of monitoring of complete cycles of freezing and thawing in hepatic cryosurgery.
For the research of the frozen liver by ultrasound in vitro [7], in combination with the modern techniques in intraoperative ultrasound, has been requested the possibility of making use of high frequency sound waves (SU ) to monitor the hepatic cryosurgery. These attempts are based on the concept that even small variations in temperature are known to alter effectively the speed of sound transmission through any means.
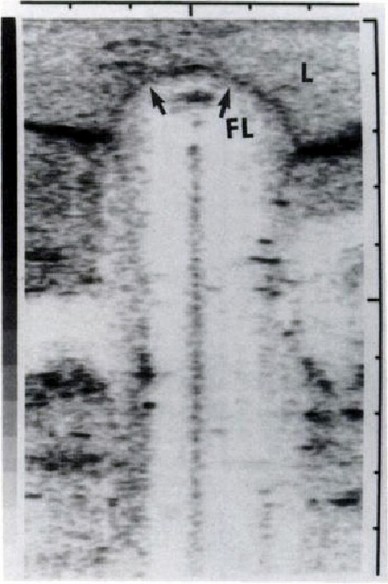 Le immagini dovute al monitoraggio con ultrasuoni del fegato sono molto eloquenti e rivelano la facilità di una comprensione e di conseguenza l’utilità che il chirurgo può trarne in sala operatoria.
Le immagini dovute al monitoraggio con ultrasuoni del fegato sono molto eloquenti e rivelano la facilità di una comprensione e di conseguenza l’utilità che il chirurgo può trarne in sala operatoria.
Il dott. Onik, come abbiamo prima detto, nel 1988 esordì con una seconda importante pubblicazione che trattava l’uso degli ultrasuoni (US) per monitorare tessuti prostatici. Detta pubblicazione aveva il seguente titolo: " US characteristics of frozen prostate ". ( Caratteristica degli ultrasuoni (US) della prostata congelata).[53] In questo lavoro l’insigne medico ricordava che la criochirurgia è già stata utilizzata con successo per il trattamento del carcinoma prostatico. Commentava, però, l’impossibilità di monitorarne il congelamento ha portato a complicazioni locali che ne hanno limitano l'uso. La monitorizzazione del processo di congelamento su animali è stata realizzata in tempo reale utilizzando gli ultrasuoni al fine di favorire gli inconvenienti sopra menzionati. Il margine del tessuto congelato è apparso come un cerchio iperecogeno con un cono d'ombra acustico posteriore. Le criolesioni scongelate hanno evidenziato un’ecogenicità marcatamente ridotta rispetto a quelle normali della prostata non gelata. Questi cambiamenti caratteristici dovrebbero consentire l'applicazione più sicura e più efficace della criochirurgia prostatica.
Onik et al. hanno dimostrato la fattibilità del monitoraggio con ultrasuoni in tempo reale (US) del volume del tessuto ghiacciato. Questa tecnica è stata utilizzata per monitorare la criochirurgia del fegato.
Miglioramenti nella transrettale US (a ultrasuoni) e la possibilità di visualizzare i tumori prostatici anche di piccole dimensioni, con US (ultrasuoni), insieme con la capacità degli US (ultrasuoni) di evidenziare il congelamento, hanno dato la possibilità di monitorare la criochirurgia prostatica transrettale con gli US, concedendo al chirurgo i vantaggi della criochirurgia senza le sue complicazioni locali.
L'obiettivo di queste ricerche è stato quello di visualizzare l'aspetto del freddo e del disgelo del tessuto prostatico con gli US. L’obiettivo è stato raggiunto permettendo di sviluppare nuove tecniche di criochirurgia per il trattamento del carcinoma prostatico [54,55].
CRYOSURGERY OF THE YEARS 90.
The 90s start with a great evolution of the cryosurgery. The studies of Dr. Onik and his collaborators have opened new and interesting perspectives on the use of the cryosurgery that still remain today.
 We note that in this decade, the century preceding to 2000 was born an active interest in the mathematical simulation of the cooling process of biological tissues and hand in hand we observe a development of mechanical and electronic instrumentation machinery responsible for cryosurgery.
We note that in this decade, the century preceding to 2000 was born an active interest in the mathematical simulation of the cooling process of biological tissues and hand in hand we observe a development of mechanical and electronic instrumentation machinery responsible for cryosurgery.
Cryosurgery captures the most interest of physicists and engineers with mathematicians and physicians who are beginning to explore these new frontiers. It is not only the biological but also the physical instrument that captures the attention of universities and research centers worldwide.
In recent years a revolution has happened similar to that created in the 60s and Lee Cooper.
Meanwhile arise schools of researchers in academia in China and Japan while the U.S. and Israeli universities give birth to brilliant ideas and new tools.
An example of this scientific awakening provides the Prof. Yoed Rabin Professor of the Department of Mechanical Engineering Tecnion-Israel Institute of Technology in Haifa with publishing a research entitled: "A New cryosurgical guide device for the controlled freezing" in 1996 [60].
In this work, the researchers YOED RABIN and AVRAHAM SHITZER present a new cryosurgical device utilizing liquid nitrogen, which is a modification of an existing trading system.
Said device is fitted with a new guide with a computer that controls the temperature of the cryogenic probe by means of an electrical heating element.
The scientific world is, at this threshold of century, aimed to determine by all the means available to the best and the most effective techniques to address and improve cryosurgery.
Many studies and past research are reviewed, revised in light of the latest scientific and technological breakthroughs.
This process of innovation, world heritage site, is still in progress. It will be our first task to describe its characteristics.
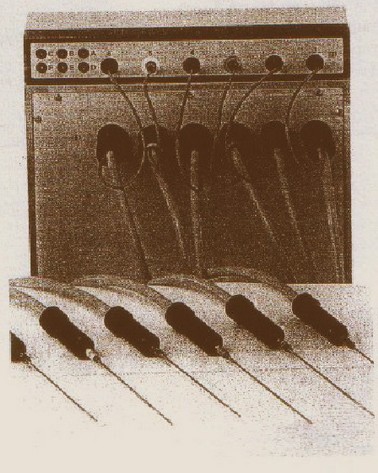
Already exists in Europe from some years a German machine of cryosurgery. Erbocrio. (Fig. O)
The characteristics of this surgical instrument are very interesting because they are designed to operate with six probes simultaneously. This allows to operate large tumors in a single surgical application. The intervention time is reduced with evident advantages of cost and health for the patient.
In this machine the probes can be sterilized and therefore can be re-used for future action.
The temperature of each of the six probes can be set and selected at will of the surgeon.
The temperatures of each probe and of the tissue are displayed on the panel by means of thermocouples. All this allows the correct positioning of the needles under control of ultrasound.
This machine operates with liquid nitrogen which is forfeited in a tank and controlled instrumentally.
START YEARS 2000s.
Scientific collaborations arise between U.S. universities and Asian, it create new schools that are undoubtedly carriers of new ideas and positive stimula.
We present then an excellent job with the title: "Numerical Simulation for Heat Transfer in Cryosurgery of the Prostate Cancer" by Jiayao Zhang, Y. Jayathi Murthy and Lisa X. Xu . (West Lafayette Shanghai).
In this work is presented an overview of the calculation to simulate the heat transfer during the freezing process in cryosurgery of the prostate cancer.
The researchers highlight the advantages of the cryosurgery in relation to other surgical techniques. They recognize that it is minimally invasive and requires low hospitalization, it results in a reduced risk of injury to normal tissue and complications. And, very importantly, is not "limited quantity" in the sense that it can be executed multiple times for recurrent cases [54].
A urethral catheter for heating, (also referred to as urethral warming), is inserted into the urethra to protect it from frost. This procedure, which was introduced by Onik [55], has reached an efficacy comparable or superior to traditional therapies in the treatment of prostate cancer [57,59,58]. Among the many advantages, however, there are limitations that affect the spread of its applications and the resulting success. The ultrasonic signals are almost completely reflected by the interface of freezing for which the acoustic shadows are present on the distal face of ice.
In addition, the temperatures of the tissue within of the iceball ( ice ball ) are unknown, because the inside cannot be monitored by ultrasound. This is a serious drawback because simply freeze the entire prostate does not necessarily provide adequate ablation.
The researchers believe that the numerical simulation provides a powerful tool to handle the complex geometries and different boundary conditions.
It is with these expressions that these scientists justify their choices and define their purpose in building a comprehensive framework for calculating numerically. To simulate the evolution of the temperature during the freezing process in cryosurgery of the prostate cancer.
In this framework , the calculation of the phase variation has been realized by a Enthalpy exchange in which is embedded the latent heat. The computational geometry has been constructed in accordance with MRI images of a real prostate, and the boundary conditions were calibrated with reference to the surfaces of the cryoprobes commercially available and used the urethral warmer.
By incorporating the geometric model and the borders have been carried out numerical simulations of the cryosurgical process itself. This allowed the display of any selected isotherm in the prostate during the cryosurgery and helped in the future perspective.
The real-time mapping of the temperature programs require computationally a more efficient and personalized thermal evolution.
The authors envisage that an optimized mesh with coarse mesh should substantially accelerate the simulation.
Another observation is that the in vivo the experimental validation of the simulation results is very important and can be aided by techniques of "imaging" advanced. The authors, with a sense of foreboding, provide for the need of creating a computationally efficient numerical solver that must be found to practically apply the optimization for the cryosurgery of prostate.
In those years, Prof Lee and collaborators had published a report whose title is very significant: "CRYOSURGERY OF PROSTATE CANCER: IMPROVEMENT USING ABLATION GLANDULAR FROM 6 TO 8 PROBES". We talked about in the chapter that deals with the biology of cold the scientific importance and biological of this work and we highlighted the importance of the base.
The researchers report that in April of 1996, an updated cryosurgical method was used using six to eight cryoprobes, and in June 1997 were treated eighty men.
This group was compared retrospectively with the last eighty cases made before of April 1996 using five cryoprobes. To ensure the homogeneity of the groups, the comparison was done with the prostate specific antigen (PSA), a clinical values, and sign Glison. Six months after cryosurgical treatment, the PSA values and epithelial residues were compared between the two groups.
The conclusions were that a method that uses eight probes has been shown to be more effective that the traditional method to five probes in glandular ablation. It was used without any difficulty, it has a wide margin of safety, and even shorter times of learning. These innovations have enabled a better approach to the objective of a complete destruction of the gland.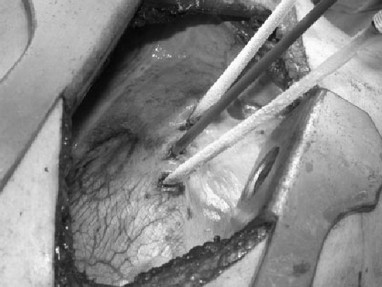 In 2006, an interesting publication of the French school on the intervention of the liver from title: "Cryosurgical Ablation Transpleurodiafragmatic for recurrent unresettable colorectal liver metastases" by the work of MATTIA STELLA, et al. proposes the interest of the school of Lyons in respect of cryosurgery [70].
In 2006, an interesting publication of the French school on the intervention of the liver from title: "Cryosurgical Ablation Transpleurodiafragmatic for recurrent unresettable colorectal liver metastases" by the work of MATTIA STELLA, et al. proposes the interest of the school of Lyons in respect of cryosurgery [70].
In this paper is described the technique of cryosurgical ablation (CSA) that allows the focal destruction of unresettable liver metastases after previous resection.
The figure P, clearly sets forth the position of the three probes and the overall theme of the intervention.
The conclusions of the French researchers about the high rate of tumor recurrence and results of the survival are a direct consequence of the severity of the disease and the treatments that patients have previously suffered. However, the French scientists repeat, the recurrence of fact is not the case with regard to the metastasis treated with CSA.
Therefore, the researchers conclude, the transpleurodiafragmatic CSA is safe and is associated with a favorable outcome in very selected patients with recurrent unresettable hepatic metastases from colorectal cancer.
In 2006 a publication of Dr. Scala et al., Head of regenerative surgery at the Department of Surgical Therapy Integrate the National Institute for Cancer Research of Genoa (Italy) [65], in which is described an intervention of cryosurgery on a patient 101 years old, suffering from advanced malignant melanoma of the skin of the face successfully managed (no recurrence two years after cryosurgical treatment).
In this article the Dr. Scala, informs that the processing was performed by means of serial cryosurgical applications (repeated cycles of freezing and thawing) that were completed within three months , moreover, that most of the lesion was treated with a cryoprobe to liquid nitrogen (-196°C) initially, while on the remaining diseased part was used a cryoprobe cooled to nitrous oxide (-89.5°C). The researcher pointed out that the intervention utilizing liquid nitrogen can freeze in substantially to greater depth while the freezing capacity of Nitrous Oxide is limited to a depth of about five millimeters. Thus, an adequate treatment of lesions require two bulky cryogenic instruments: one with liquid nitrogen for bulky tumors, due to the more pronounced vascular supply, and then for obtain a greater depth of infiltration into the surrounding tissues and nitrous oxide for the residual superficial disease.
Another interesting observation of the scholar is to use more aggressiveness on the tumor to produce an "ice ball" including at least 5 mm of apparently normal tissue surrounding the primary tumor.
We will present in the next chapter, to a series of interventions Cryosurgical of skin cancers accompanied by details and images of these interventions carried out by Dr. Scala.
We shall show therefore only some elements of the Italian probes that the surgeon uses in his operations. (Fig. Q).
The Dr. M. Scala observes which in the future we will needs surgery where the machines will have to answer to the surgeons. He hopes first of all in the regularity of operation that must be able to allow for variability of the depth of the front cryogenic according to the need of a mathematics "simulation". A conversation between the machine and surgeon so that the surgeon can know in advance regarding the effects of the cryogenic front. In other words, the intervention "simulated or virtual ".
Among the final awakening of cryosurgery and the general interest in it of the various surgeons in the world we present a study of effective application of the cryosurgery to very painful disorder of the foot: fasciitis.
The Doctors Brian H. Allen, Lawrence M. Fallat, and Steve M. Schwartz published an article entitled "Cryosurgery: an innovative technique for the treatment of plantar fasciitis". These are the years of 2007 and almost all of the most renowned universities of the world had studied and applied the cryosurgery. In this prospective study whose objective is to test the efficacy of cryosurgery on the heel. The plantar fasciitis is a common foot problem seen often by a variety of medical specialties.
Were treated fifty-nine patients (61 heels), who had failed conservative therapy and were considered candidates for cryosurgery. Patients were rated on a 11-point visual analog scale assessed before surgery and followed up to one year follow-up. Where zero is no pain and 10 is the state of worse pain I've ever had. Pain was assessed on the day of surgery and in subsequent 1, 7, 28, 90, 180 and 365 after the procedure cryosurgery.
The mean pain score was 8:38 ascertained prior to cryosurgery on day zero, is statistically significant as a reference for the assessment of average pain, equals 1.26 at 365 days after surgery.
The percutaneous denervation was administered to 61 heels involving 59 patients with instrumentation Cryotech Corporation ( Atlanta, GA) (Fig. R and S) in an outpatient study.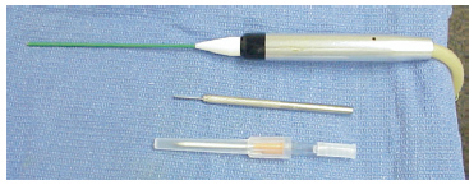
efore the procedure, the area of maximum tenderness was been carefully identified (Fig. S). The most common place for this was the palpable tenderness along the medial band of the plantar fascia originates near the calcaneal tubercle [56]. These results suggest that cryosurgery is significantly effective in the treatment of patients with recalcitrant plantar fasciitis. The cryosurgery offers a very effective way of treatment after failure of conservative process without resorting to invasive surgery outpatient. Additionally, cryosurgery for the treatment of plantar fasciitis includes a minimum period of recovery with fewer complications. The end result seems to be similar to any surgical correction with minimal or no disability and no additional medical expenses. A direct comparison of outpatient surgery compared to the cryosurgery could prove invaluable.
These results suggest that cryosurgery is significantly effective in the treatment of patients with recalcitrant plantar fasciitis. The cryosurgery offers a very effective way of treatment after failure of conservative process without resorting to invasive surgery outpatient. Additionally, cryosurgery for the treatment of plantar fasciitis includes a minimum period of recovery with fewer complications. The end result seems to be similar to any surgical correction with minimal or no disability and no additional medical expenses. A direct comparison of outpatient surgery compared to the cryosurgery could prove invaluable.
As we have previously stated the cryosurgery, although with the special restrictions, in the late 2010s, has been applied in many parts of the world (and successfully).
We see, in fact, that Norwegian surgeons, using equipment built in northern Europe, have ventured in the interventions of cryosurgery of the prostate cancer.
In 2007, the Dr. Johansen TE Bjerklund of the Urology section, Telemark Hospital, Porsgrunn, Norway presented a paper describing an intervention of cryosurgery of the prostate cancer [61].
The objective of this work was to present the preliminary experience with the CSA ( prostate cryotherapy ablation ) in prostate cancers in the hospital of Norway.
The team of ultrasound instruments was a B & K Falkon 2101 with a 8658 ( B6K Danish) probe. There it was a pedal and a braqui standoff in the probe (Fig. T). The braqui standoff was a plastic sheet placed around the probe with a window for the expansion of the internal manifold when we want to heat with water. To freeze they utilized argon gas and helium. Most of the work was done with epidural or general anesthesia so that the patient could not move. The treatment of CSA, including the insertion of needles and their period of freezing and heating was carried out as described above and in accordance with the clinical guidelines of the European Association of Urology (EAU ) of prostate cancer [63].
Most of the work was done with epidural or general anesthesia so that the patient could not move. The treatment of CSA, including the insertion of needles and their period of freezing and heating was carried out as described above and in accordance with the clinical guidelines of the European Association of Urology (EAU ) of prostate cancer [63].
The Norwegian surgeon says, Cryosurgical after the interventions and the appropriate statistical analysis, that the CSA is recognized by the UAE, now, as a viable therapeutic option for the treatment of prostate cancer. Confirms that many institutions offer the only CSA in elderly patients due to the lack of long-term results and that if the long-term results confirm those obtained within a short time, the CSA may be offered as a primary treatment even in young patients.
In 2011 was published an article whose title, very significant, "Cryotherapy for Barrett's Esophagus: Who, How, and Why ? " which highlights the need to understand the issues of cancer of the esophagus about the cryosurgery.
That article was written by Dr. Ann Chen and Dr. P. Jay Pasricha who is the inventor of the device Polar Wand cryoablation ( Gl Power, Camp Hill, Pennsylvania, we will present in the following) and a consultant for the company.
These researchers of the Division of Gastroenterology and Hepatology , Stanford University School of Medicine , Stanford University Medical Center , Redwood City, United States of America present the challenges and benefits of a particular cryosurgery : the esophagus .
It’s need to remember that to approximately 16,500 Americans have been diagnosed with esophageal cancer and 14,500 of them die from this cancer each year [68]. The incidence of esophageal adenocarcinoma has continued to grow dramatically over the last four decades and is growing at a faster rate than any other cancer in the United States. The Barrett's esophagus (BE ) is a known risk factor in the development of esophageal adenocarcinoma.
With the presence of high-grade dysplasia ( HGD), however, the risk of progression to cancer can be of the value of 10% per patient - year. Traditionally , the surgery with esophagectomy has been the mainstay of treatment for patients with HDG , however, many of these are older, and are considered poor candidates for surgery . Esophagectomy is also associated with a significant mortality and morbidity, and recent reports have shown recurrence of Barrett's metaplasia in 18% of patients after esophagectomy " curative", despite high doses of medical acid suppressive [69] .
THE ENDOSCOPICAL DEVICES OF THE CRYOTHERAPY.
From what we have got to check the development of the "techniques of cold " has consistently followed the technological progress that is related to scientific and technological discoveries.
The evolution of physical, medicine and engineering goes hand in hand and, as we shall see in next chapter, one tied to each other.
A final example of how past experiences have become the heritage of the actual surgery, we present a series of works that testify to the true vision of Dr. Fay in regard to this technique that collects great success and is still in a continuous surgical and technological progress.
The Hypothermia already introduced in 1938 by Dr. Fay has developed and honed cryogenic surgical techniques and of instrumentation.
At the end of the year 2010 in the world is successfully practiced on young subjects and no.
In 2010, the Doctors Gunasekaran G, K Bencsath, Hupertz V, Fung JJ, Pettersson G, Miller C. the Cleveland Clinic Foundation, Cleveland, Ohio USA recorded an intervention of deep hypothermia with circulatory arrest on a child to help the management of stenosis of the vena cava as a result of an intervention by the liver. The results were satisfactory [71].
The following year the Russian team led by Dr. Kazanskaia GM et al. describe the benefits of the hypothermia applied to children with the disease of Roger [72].
In 2011, many international universities such as Northern Ireland in an article written by Doctors Parissis H, Hamid U, Soo A, Al- Alao B. treating systemic hypothermia for the protection of the central nervous system during surgery has revealed questions and doubts on this instrument [73]. While the Doctors Krüger T, Weigang E, Hoffmann I, Blettner M, H Aebert, the GERAADA Investigators (GERMANY ) describe the cerebral protection during surgery for acute type A aortic dissection: results from the registry for the German type of aortic dissection [74]. In the same year University of the Malaysia [75] Belgium [76] present their work regarding hypothermia, highlighting the undeniable advantages.
In 2012 there are countless actions undertaken in the world. The United States is presented with several aortic operations with hypothermic circulatory arrest [77-81]. Also from Greece comes to us, in that year, a publication of aortic surgery with hypothermic circulatory arrest [82]. And two works from Japan, always on the same subject [83,84], they propose a research on the improvement of the evoked potential monitoring during surgery of the thoracic aorta in hypothermia [85].
In the University of Bologna in Italy Prof. D. Pacini et al. has showed a publication entitled "selective antegrade cerebral perfusion and moderate hypothermic aortic arch surgery: clinical outcomes in elderly patients" [86].
A few months away from China is presented an experimental work on studying the security of a rabbit with cerebral circulatory arrest [87] while the professors Ji B , Liu J , Wang X , C Long , Chineses, present the issue of security [88]. The same theme is proposed by the team of the German professors Zierer A, Moritz A. which investigate the cerebral protection for aortic arch surgery by adopting a mild hypothermia with selective cerebral perfusion [89].
In 2012 at Siena in Tuscany (Italy) was carried out an operation on a child whose body temperature was lowered to 18 degrees Celsius.
Surgeons of "delle Scotte" Hospital in Siena stopped his heart for 15 minutes and started the surgery to remove an big aneurysm from his brain.
The child after a short stay in the ICU Neurosurgery, is admitted in Pediatric Neurosurgery, he's fine.
FUTURE OF CRYOSURGICAL EQUIPMENTS.
To Estimate in advance the future development of the cryosurgical instrumentation is very difficult if not almost impossible. We will try, however, to draw the general guidelines useful to us serving us of both modern scientific and technological discoveries. Discoveries which may, in our opinion, be indicative of future trends of this science.
Are three, in our opinion, the key roads that lead to a very advanced instrumentation of the cryosurgery (excluding surgery and new discoveries in the biology of the cold):
1) development of refrigeration systems.
2) creation of new software for the simulation of the fronts of freeze in biological tissues.
3) Flexible devices and self-managed.
1 ) Future development of refrigeration systems .
The techniques of the cold.
Recall that the basic concepts of the gas refrigerators are, in our case, an aid in the study of modern techniques and future. The Joule-Thompson effect, widely used in cryosurgery, is the basic phenomenon for the understanding of modern apparatuses of Cryosurgical and it will be in a specific chapter of the our study.
We will treat in a special paragraph the description of the refrigeration systems, namely those defined emerging free-piston impulse wave and the Peltier cells which represent the cryogenic solid state.
2 ) Creation of new simulation software fronts progress cryogenic biological tissues .
This work was carried out by the Faculty of Mathematics, University of Genoa (Italy). The researchers Giovanni Giorgi, Leopoldo Avalle, Massimo Brignone, Michele Piana and Giacomo Caviglia present a very special approach that anticipates its kind , the report processing data in the future of the cryosurgery [64].
This procedure that we can define cryosurgical planning has as objective to establish the best positions of the cryoprobes and of the temperature sensors and calculate their number as a function of structural topology and the temperature and duration of the freezing process.
The processing logic uses the procedure optimizing ACO (Ant Colony Optimization = optimization of ant colonies ) under which the calculation is expressed in terms of direct costs it means by numerically solving various problems of Stefan.
ACO is inspired by the way ants find and bring the food to their nest. While an ant is returning to the nest after taking a little food, it releases a pheromone trail: this serves as a path for the ants nearby, which are able to reach the food from the detection of the pheromone.
The behavior of ants is paraphrased in ACO that identifies the cost function F with the length of the path to the food, and the traces of pheromone with a probability density that is updated at each iteration that depends on the value of the cost function for a set of states.
ACO defines, therefore, a probability distribution that is more dense in correspondence of the states less expensive.
In conclusion, the processing system according to the parameters specified above identifies, in an optimal way, the ideal number of probes and their location in the tissues.
This work is certainly not ended because it has been studied in two-dimensional space, but the road is traced and the prospects within a short time will lead to the resulting three-dimensional extension.
To regard to the processing of data with reference to cryosurgery in recent years there has been a great interest on the part of the Americans University, Japanese, Israeli to mention only the most important and active.
Take, as an example, the work of the professors Daigo Tanaka, Kenji Shimada, Michael R. Rossi and Rabin Yoed in the department of mechanical engineering and biomechanics of Carnegie Mellon University, Pittsburgh, PA, USA [62].
This brief overview of publications on cryosurgery whose content has a tendency to improve and facilitate the activities of doctors should be seen as a whole and ideally add any contribution to the ultimate objective whose purpose is the development of an cryogenic instrument very operating.
3)The equipment cryogenic multi flexible and self-managed .
We expect that in the near future will be built machines for cryosurgery completely free from human dexterity.
The presence of the surgeon will always be important but its role must be of controller and to do supervision to the operations. His contribution manual, necessary and useful, will be required in all those operations that the machine is not able to perform.
The cold will be produced completely independently. Simply insert the plug into the electrical outlet, and after a little time it will be reached the temperatures to operate. The machine will have generated the low cryogenic temperatures on the probes. The surgeon will chose the temperatures according to the biological nature of the intervention.
The biological and radiological information will be provided to the surgical staff and will show all the parameters that characterize the intervention protocols. These protocols, improved and adapted to the new structures, will be stored in the computer system that will be supplied with each cryogenic machine.
The work of the surgeon begins with a study of radiographic and a "dialogue" with the computer that owns the machine. It is this the introductory phase that helps him in the cryogenic activity without the presence of the patient. The physician plays a role of utmost importance and indispensable, his personal experiences will be confronted with the vision of the physical and biological phenomena that are offered on the board monitor.
After these activities, the parameters will be "saved" from the processing system. The real operation will be made in compliance with the protocol.
For us this will be the new frontier of cryosurgery. Multi flexible machines and almost self-managed, will be equipped with powerful computing devices and specific software and refined intervention in collaboration with the medical staff.
BIBLIOGRAPHY |
|
1 |
Schreuder HWB, ed.The cryosurgical treatment of benign and low-grade malignant bone tumors. Wageningen, The Netherlands: Ponsen&Looijen; 1997:7–11 |
2 |
Breasted JH. The Edwin Smith surgical papyrus. Vol III. Chicago: University of Chicago, Oriental Institute Publications; 1930:72–73 |
3 |
Dawber RPR. Cold kills! Clin Exp Dermatol 1988;13:137–150. |
4 |
Davison MHA. The evolution of anesthesia. Br J Anaesth 1959;31:134–137 |
5 |
Larrey DJ. Surgical memoirs of campaigns of Russia, Germany and France.Translation by JCMercer. Philadelphia: Carey and Lea; 1832:7–11 |
6 |
Gage AA. History of cryosurgery. Semin Surg Oncol 1998;14: 99–109 |
7 |
Arnott J: Practical illustrations of the remedial efficacy of a verylow or anaesthetic temperature. I. In cancer. Lancet 1850; 2: 257–259 |
8 |
Bird HM: James Arnott, M.D. (Aberdeen) 1797-1883: a pioneer in refrigeration analgesia. Anaesthesia 1949; 4:10–17 |
9 |
White AC: Liquid air: its application in medicine and surgery. Med Rec 1899; 56:109–112 |
10 |
Pusey WA: The use of carbon dioxide snow in the treatment of nevi and other lesions of the skin. J Am Med Assoc 1907; 49:1354–1356. (da eliminare uguale a 18) |
11 |
Torre D, Lubritz RR, Kuflik EG. Practical cutaneous cryosurgery. Norwalk, CT: Appleton & Lange, 1988. |
12 |
Sealy WC, Brown IW Jr, YoungWGJr (1958)A report on the use of both extracorporeal circulation and hypothermia for open heart surgery. Ann Surg 147: 603–613 |
13 |
Solomon RA, Smith CR, Raps EC, Young WL, Stone JG, Fink ME (1991) Deep hypothermic circulatory arrest for the management for complex anterior and posterior circulation aneurysms. Neurosurgery 29: 732–737 |
14 |
Spetzler RF, Hadley MN, Rigamonti D, Carter LP, Raudzens PA, Shedd SA, Wilkinson E (1988) Aneurysms of the basilar artery treated with circulatory arrest, hypothermia, and barbiturate cerebral protection. J Neurosurg 68: 868–879 |
15 |
Wolf JM. Temple Fay, M.D.—Inquisitive scientist, prolific scrivener. Pathol Med J 1965;68:47—51. |
16 |
Fay T (1959) Early experiences with local and generalized refrigeration of the human brain. J Neurosurg 16: 239–260. |
17 |
Zacarian SA, Adham MI: Cryotherapy of cutaneous malignancy. Cryobiology 1966; 2:212–218. |
18 |
Cooper IS, Lee A: Cryostatic congelation: a system for producing a limited controlled region of cooling freezing of biologic tissues. J Nerv Ment Dis 1961; 133:259–263. |
19 |
Yantomo C, Soanes WA, Gonder MJ, Shulman S: Studies in cryoimmunology. I. The production of antibodies to urogenital tissue in consequence of freezing treatment. Immunology 1967; 12:395–410. |
20 |
Gonder MJ, SoanesWA, Smith V. Chemical and morphologic changes in the prostate following extreme cooling. Ann NY Acad Sci 1965;125:716–729 |
21 |
Ortved WE, O’Kelly FM, Todd IA, et al: Cryosurgical prostatectomy: a report of 100 cases. Br J Urol 1967; 39:577–583. |
22 |
Jordan WP Jr, Walter D, Miller GH Jr, Drylie D: Cryotherapy of benign and neoplastic tumors of the prostate. Surg Gynecol Obstet 1967; 125:1265–1268. |
23 |
Dowd, JB, Flint LD, Zinman LN, Tripathi VN: Experiences with cryosurgery of the prostate in the poor-risk patient. Surg Clin North Am 1968; 48; 627–632. |
24 |
Rouvalis P: Cryosurgery of the prostate under local anesthesia. J Urol 1969; 102:244–245. |
25 |
Flocks RH, Nelson CM, Boatman DL: Perineal cryosurgery for prostatic carcinoma. J Urol 1972; 108:933–935. |
26 |
Torre D: Alternate cryogens for cryosurgery. J Dermatol Surg 1975; 1:56–58 |
27 |
Soanes, W.A., Gonder, M. J. and Ablin, R. J. : Immuno-cryothermic response. Read at annual meeting of Society of Cryosurgery, Miami Beach, Florida, January 12-17, 1969. |
28 |
Stellar S: Intracranial cryosurgery in a canine model: a pilot study [1etter]. Surg Neurol 1993; 39:331–332. |
29 |
Conway LW: Stereotaxic diagnosis and treatment of intracranial tumors including an initial experience with cryosurgery for pinealomas. J Neurosurg 1973; 38; 453–460. |
30 |
Walder HA: Experimental cryosurgery. In von Leden H, Cahan WG (eds): “Cryogenics in surgery’’ Flushing, NY: Medical Examination Publishing; 1971. p. 150–181. |
31 |
Soanes WA, Ablin RJ, Gonder MJ: Remission of metastatic lesions following cryosurgery in prostatic cancer: immunologic considerations. J Urol 1970; 104:154–159. |
32 |
Gursel E, Roberts M, Veenema R: Regression of prostate cancer following sequential cryotherapy to the prostate. J Urol 1972; 108:928–932. |
33 |
Gage AA: Cryosurgery for difficult problems in cutaneous cancer. Cutis 1975; l6:465–470. |
34 |
Zacarian SA (ed): “Cryosurgical advances in dermatology and tumors of the head and neck. Springfield, IL: Charles C. Thomas; 1977. |
35 |
Torre D, Lubritz R, Graham G: Cryosurgical treatment of basal cell carcinomas. Prog Dermatol 1978; 12:11–16. |
36 |
Shields JA, Parsons H, Shields CL, Gibson ME: The role of cryotherapy in the management of retinoblastoma. Am J Ophthalmol 1989; 108:260–264. |
37 |
Jakobiec FA, Rini FJ, Fraunfelder FT, Brownstein S: Cryotherapy for conjunctival primary acquired melanosis and malignant melanoma. Experience with 62 cases. Ophthalmology 1988; 95:1058–1070. |
38 |
Townsend DE, Richart RM: Cryotherapy and carbon dioxide laser management of cervical intraepithelial neoplasia: a controlled comparison. Obstet Gynecol 1983; 61:75–78. |
39 |
Creasman WT, Hinshaw WM, Clarke-Pearson DL: Cryosurgery in the management of cervical intraepithelial neoplasia. Obstet Gynecol 1984; 63:145–149. |
40 |
Ferenczy A: Comparison of cryo- and carbon dioxide laser therapy for cervical intraepithelial neoplasia. Obstet Gynecol 1985; 66:793–798. |
41 |
Benedet JL, Miller DM, Nickerson KG, Anderson GH: The results of cryosurgical treatment of cervical intraepithelial neoplasia at one, five, and ten years. Am J Obstet Gynecol 1987; 157:268–273. |
42 |
Andersen ES, Thorup K, Larsen G: The results of cryosurgery for cervical intraepithelial neoplasia. Gynecol Oncol 1988:30:21–25. |
43 |
Sumida S, Okuyama Y, Kamegai T. Serum hepatitis from frozen blood. Lancet 1967;II:1255–1256. |
44 |
Sumida S, Sumida M, Miyata K, et al. Frozen blood: HLA sensitization. Low Temp Med 1975;1:227–231. |
45 |
Sumida S, Eto S, Yamaguchi A, Kawata H. Fibrillation and contraction tracings from adult rat hearts after freezing in liquid nitrogen for ten years. Low Temp Med 1984;10:47–51. |
46 |
Sumida S, Xi Y, Oshikawa K. How long can we cryopreserve stem cells of cancer patients? Cryobiology 1997;35:334. |
47 |
Sumida S. Terminology of low temperature in medicine and cryobiology. Low Temp Med 2002;28:49–50. |
48 |
Sumida S. Transfusion of blood preserved by freezing. Stuttgart: Lippincott-Geroge Thieme; 1973:8–21. |
49 |
Sumida S, Ebine K,Tamura S, Lee M. Viability of supercooled hearts for transplantation. Cryobiology 1987;24:570–671. |
50 |
Bonney WW, Fallon B, Gerber WL, et al: Cryosurgery in prostatic cancer: survival. Urology 1982; 19:37–42. |
51 |
Loening S, Lubaroff D: Cryosurgery and immunotherapy for prostatic cancer [Review]. Urol Clin North Am 1984; 11:327–336. |
52 |
Onik G, Gilbert J, Hoddick W, et al: Sonographic monitoring of hepatic cryosurgery in an experimental animal model. AJR Am J Roentgenol 1985; 144:1043–1047. |
53 |
Onik G, Cobb C, Cohen J, et al: US characteristics of frozen prostate. Radiology 1988; 168:629–631. |
54 |
Onik, G. M., 1995, “Prostate Cryoablation: A Reappraisal,” Percutaneous Prostate Cryoablation, G. M. Onik, B. Rubinsky, G. Watson, R. J. Ablin, eds., Quality Medical Publishing, St. Louis, MO, Chap. 1. |
55 |
Onik, G., 1989, “Transperineal Prostatic Cryosurgery Under Transrectal Ultrasound Guidance,” Semin. Interventional Radiol., 6, pp. 90–96. |
56 |
Kinley S, Frascone S, Calderone D, Wertheimer SJ, Squire MA, Wiseman FA. Endoscopic plantar fasciotomy versus traditional heel spur surgery: a prospective study. J Foot Ankle Surg 32:595– 603, 1993. |
57 |
Balm DK, Lee F, Solomon MH, et al: Prostate cancer: US-guided percutaneous cryoablation. Radiology 1995; 194:551–556. |
58 |
Ghafa, M. A., Johnson, C. W., Taille, A. D. L., Benson, M. C., Bagiella, E., Fatal, M., Olsson, C. A., and Katz, A. E., 2001, “Salvage Cryotherapy Using an Argon Based System for Locally Recurrent Prostate Cancer after Radiation Therapy: The Columbia Experience,” J. Urol. [Baltimore], 166, pp. 1333–1338. |
59 |
Bahn, D. K., Lee, F., Badalament, R., Kumar, A., Greski, J., and Chernick, M., 2002, “Target Cryoablation of the Prostate: 7-Year Outcomes in the Primary Treatment of Prostate Cancer,” Urology, 60s2ad, pp. 3–11. |
60 |
Yoed Rabin, Avraham Shitzer. A new Cryosurgical Device for Controlled Freezing. Cryobiology 1996; 33: 82-92. |
61 |
Bjerklund Johansen TE. Crioterapia pròstatica como tratamiento primario en pacientes con càncer de prostata. Actas Urol Esp. 2007; 31(6): 651-659. |
62 |
Daigo Tanaka, Kenji Shimada, Michael R. Rossi, Yoed Rabin. Towards intra-operative computerized planning of prostate cryosurgery. International Journal of medical Robotics and Computer Assisted Surgery 2007; 3: 10-19. |
63 |
Cytron S, Greene D, Witsch UKF, Nylund P, Bjerklund Johansen TE. Cryoablation of the prostate: Technical recommendations. Accepted for publication as part of EAU guidelines on prostate cancer. European Association of Urology. Guidelines 2007 (ISBN-13:978-90-70244-59-0). |
64 |
Giovanni Giorgi, Leopoldo Avalle, Massimo Brignone, Michele Piana and Giacomo Caviglia. An optimization approach to multiprobe cryosurgery planning. Computer Methods in Biomechanics and Biomedical Engineering May 2011; 00: 1–14. |
65 |
Scala M., Gippone M., Queirolo P., et al. Cryosurgery for advanced malignant melanoma of the facial skin. A case of report. In Vivo 2006; 20: 153 – 156. |
66 |
H. Wang, W. Olivero, D. Wang, and G. Lanzino. History of Neurosurgery. Cold as a therapeutic agent. Acta Neurochir (Wien) 2006; 148: 565-570. |
67 |
Rubinsky B.. Cryosurgery. Ann. Rev. Biomed. Eng. 2000; 2: 157-187. |
68 |
American Cancer Society. Cancer facts and figures 2009. Atlanta (GA): American Cancer Society; 2009. |
69 |
Wolfsen HC, Hemminger LL, DeVault KR. Recurrent Barrett’s esophagus and adenocarcinoma after esophagectomy. BMC Gastroenterol 2004;4:18. |
70 |
Mattia Stella, François Mitieux, Pierre Meeus, Pierre kaemmerlen, Cyril Lafon, Michel Rivoire. Transpleurodiaphragmatic Cryosurgical Ablation for Recurrent Unresectable Colorectal Liver Metastases. Journal of Surgical Oncology 2006; 93: 268-272. |
71 |
Gunasekaran G, Bencsath K, Hupertz V, Fung JJ, Pettersson G, Miller C. Deep ypothermia with circulatory arrest to aid in the management of suprahepatic vena cava stenosis after liver transplantation. Liver Transpl. 2010 Dec;16(12):1434-6. doi: 10.1002/lt.22183. |
72 |
Kazanskaia GM, Volkov AM, D'iakonitsa TM, Karas'kova AM. [Ultrastructure of coronary microvessels in conditions of heart reperfusion following prolonged ischemia while applying various methods of artificial hypothermia]. Tsitologiia. 2011;53(12):968-77. |
73 |
Parissis H, Hamid U, Soo A, Al-Alao B. Brief review on systematic hypothermia for the protection of central nervous system during aortic arch surgery: a double-sword tool? J Cardiothorac Surg. 2011 Nov 20;6:153. doi: 10.1186/1749-8090-6-153. |
74 |
Krüger T, Weigang E, Hoffmann I, Blettner M, Aebert H. Circulation. Cerebral protection during surgery for acute aortic dissection type A: results of the German Registry for Acute Aortic Dissection Type A (GERAADA). 2011 Jul 26;124(4):434-43. |
75 |
Sachithanandan A, Badmanaban B. Re-do sternotomy for complex aortic surgery under deep hypothermic circulatory arrest: left ventricular vent--an invaluable adjunct. Interact Cardiovasc Thorac Surg. 2011 Apr;12(4):608. |
76 |
El Oumeiri B, Louagie Y, Buche M. Reoperation for ascending aorta false aneurysm using deep hypothermia and circulatory arrest. Interact Cardiovasc Thorac Surg. 2011 Apr;12(4):605-8. |
77 |
Khalpey Z, Dekkers RJ, Nauta FJ, Shekar P. Warm beating heart with deep hypothermic circulatory arrest: a technique for an unclampable aorta with aortic valve regurgitation. J Thorac Cardiovasc Surg. 2012 Sep;144(3):731-2. |
78 |
de Zélicourt D, Jung P, Horner M, Pekkan K, Kanter KR, Yoganathan AP. Cannulation strategy for aortic arch reconstruction using deep hypothermic circulatory arrest. Ann Thorac Surg. 2012 Aug;94(2):614-20. |
79 |
Corvera JS, Fehrenbacher JW. Open repair of chronic aortic dissections using deep hypothermia and circulatory arrest. Ann Thorac Surg. 2012 Jul;94(1):78-81; discussion 82-3. |
80 |
Mazzeffi M, Marotta M, Lin HM, Fischer G. Duration of deep hypothermia during aortic surgery and the risk of perioperative blood transfusion. Ann Card Anaesth. 2012 Oct-Dec;15(4):266-73. |
81 |
Di Luozzo G, Griepp RB Cerebral protection for aortic arch surgery: deep hypothermia. Semin Thorac Cardiovasc Surg. 2012 Summer;24(2):127-30. |
82 |
Perreas K, Samanidis G, Dimitriou S, Kalogris P, Balanika M, Antzaka C, Khoury M, Michalis A. Outcomes after ascending aorta and proximal aortic arch repair using deep hypothermic circulatory arrest with retrograde cerebral perfusion: analysis of 207 patients. Interact Cardiovasc Thorac Surg. 2012 Sep;15(3):456-61. |
83 |
Hata M, Akiyama K, Wakui S, Takasaka A, Shiono M. Concomitant aortic valve and ascending aorta replacement with moderate hypothermic circulatory arrest to treat an aortic bicuspid valve with post-stenotic dilatation. Surg Today. 2012 Sep;42(9):913-6. |
84 |
Hiraoka K, Kawatsu S, Mori E, Saiki Y. Total aortic arch replacement using hypothermic circulatory arrest with antegrade selective cerebral perfusion: are there cerebral deficits other than frank stroke?. Gen Thorac Cardiovasc Surg. 2012 Jun;60(6):345-9. |
85 |
Kawaguchi M, Kawamata M, Yamada Y. Improvement of motor evoked potentials monitoring is required during thoracic or thoracoabdominal aortic aneurysm surgery under hypothermic cardiopulmonary bypass. J Anesth. 2012 Apr;26(2):157-9. |
86 |
Pacini D, Di Marco L, Leone A, Di Bartolomeo R, Sodeck G, Englberger L, Carrel T, Czerny M. Antegrade selective cerebral perfusion and moderate hypothermia in aortic arch surgery: clinical outcomes in elderly patients. Eur J Cardiothorac Surg. 2012 Aug;42(2):249-53; discussion 253. |
87 |
Wang Q, Yang J, Long C, Zhao J, Li Y, Xue Q, Cheng L, Cheng W. Hyperoxia management during deep hypothermia for cerebral protection in circulatory arrest rabbit model. ASAIO J. 2012 Jul-Aug;58(4):330-6. |
88 |
Ji B, Liu J, Wang X, Long C. How much is safe: the flow of antegrade cerebral perfusion during deep hyperthermia circulatory arrest. Ann Thorac Surg. 2012 Feb;93(2):693-4. |
89 |
Zierer A, Moritz A. Cerebral protection for aortic arch surgery: mild hypothermia with selective cerebral perfusion. Semin Thorac Cardiovasc Surg. 2012 Summer;24(2):123-6. |